Covid 19
About COVID-19
COVID-19 is a highly contagious virus that mainly attacks the lungs. It is transmitted through droplets created from sneezing and coughing from those infected. The virus enters the body via the nose, mouth and eyes. After acute COVID-19 illness, recovered patients may continue to report a wide variety of signs and symptoms including fatigue, body ache, cough, sore throat, difficulty in breathing, etc.
A holistic approach is required for follow up care and well-being of all post-COVID recovering patients.COVID-19 affects different people in different ways. Most infected people will develop mild to moderate illness and recover without hospitalization.
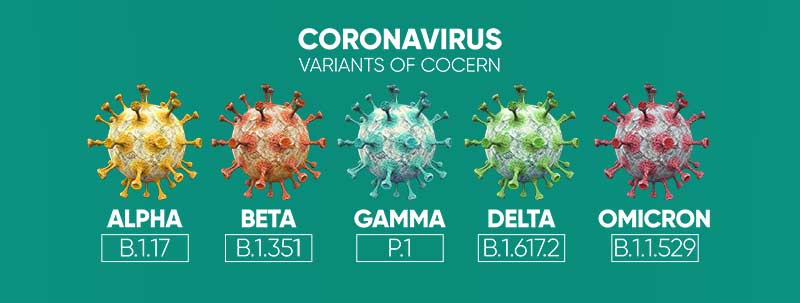
It is the largest category for an RNA virus. In most cases, it is difficult to detect if coronavirus or a different cold-causing virus is causing you fever.
Known as “COVID-19”, the newly identified corona virus can cause pneumonia, and like other respiratory infections, it has an incubation of between 1 and 14 days.
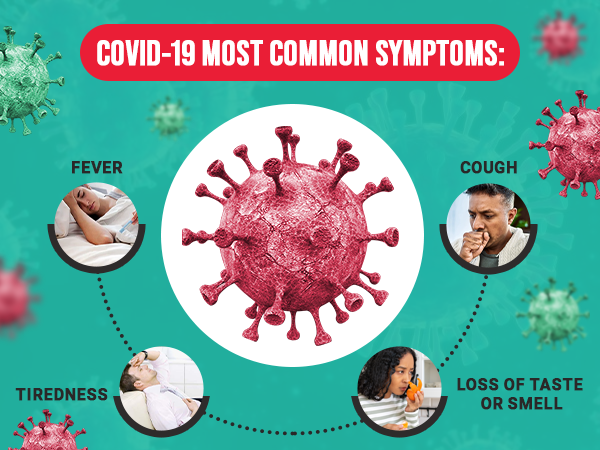
Most common symptoms:
- Fever
- Cough
- Tiredness
- Loss of taste or smell
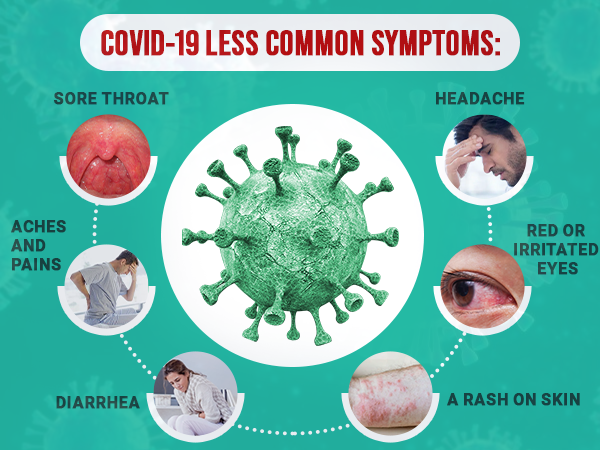
Less common symptoms:
- Sore throat
- Headache
- Aches and pains
- Diarrhea
- A rash on skin, or discoloration of fingers or toes
- Red or irritated eyes
COVID-19: HOW IT SPREADS
COVID-19 is an infectious disease caused by the recently discovered corona virus. The COVID-19 virus spreads primarily through droplets of saliva or discharge from the nose when an infected person coughs or sneezes. The virus enters the body via nose, mouth and eyes. Some recent studies suggest that the virus may be air borne and could be spread through fine infected droplets that remain suspended in the air in closed air-conditioned environments due to absence of cross-ventilation, even when you are not in direct contact with an infected person
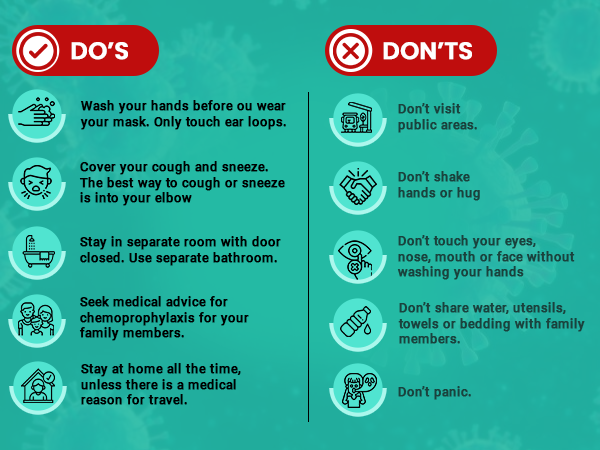
REDUCING TRANSMISSION
- Staying at home if possible, especially individuals > 60 years or less than 5 years of age, or those having co- morbidities like diabetes, hypertension or chronic ailments. Avoid meeting visitors at home.
- Washing your hands and face at regular intervals with soap and water.
- Wearing a mask at all times when out of the house.
- Social distancing – Keeping a distance of 6 feet from others when out of the house.
- Cleaning frequently touched surfaces with disinfectant regularly.
- Avoiding closed spaces with central air-conditioning like offices, malls, etc. with inadequate fresh air.
- Avoiding physical contact sick people.
HOW IT MANIFESTS
Commonly reported symptoms of COVID-19
- Dry cough, cold, sore throat.
- Fever or chills.
- Fatigue, tiredness, muscle or body aches.
- Headache.
- Congestion or runny nose.
- Shortness of breath or difficulty breathing.
- Loss of appetite/ taste/smell.
The severity and duration of symptoms for people who have COVID-19 can vary; for most people, usually the symptoms take 7-14 days to subside. Some people may have no symptoms while others may require hospitalization to treat these symptoms. Recovery from symptoms varies from person to person. In some cases, these symptoms might persist even after testing negative for COVID-19. If you have any of these symptoms, you should consult your physician who may advise for COVID testing. If you test positive and have mild symptoms, the doctor may advise home treatment. Else, hospitalization may be advised. Every positive test result is also informed to government and government representatives may visit your house or call for checking on you and isolating the family members.
COVID-19: HOMECARE
When to seek emergency medical care
- Oxygen Saturation – Less than 94%.
- Respiratory Rate – More than 24 breaths per minute.
- Fever – Persistent fever despite oral steroids beyond 7 days.
- Blood Pressure – Systolic BP: Below 100 mmHg or Above 180 mmHg Diastolic BP: Below 60 mmHg or Above 110 mmHg.
- Any other critical symptom.
Instructions for caregivers
Mask: The caregiver should wear a triple layer medical mask appropriately when in the same room with the ill person. Front portion of the mask should not be touched or handled during use. If the mask gets wet or dirty with secretions, it must be changed immediately. Discard the mask after use and perform hand hygiene after disposal of the mask.
Hand hygiene: must be ensured following contact with ill person or his immediate environment. Hand hygiene should also be practiced before and after preparing food, before eating, after using the toilet, and whenever hands look dirty. Use soap and water for hand washing at least for 40 seconds. Alcohol-based hand rub can be used, if hands are not visibly soiled. After using soap and water, use of disposable paper towels to dry hands is desirable. If not available, use dedicated clean cloth towels and replace them when they become wet.
Exposure to patient: Avoid direct contact with body fluids of the patient, particularly oral or respiratory secretions. Use disposable gloves while handling the patient. Perform hand hygiene before and after removing gloves.
Avoid exposure to potentially contaminated items in the patient’s immediate environment (e.g. avoid sharing utensils, dishes, used towels or bed linen).
Food must be provided to the patient in his room.
Utensils and dishes used by the patient should be cleaned with soap/detergent and water wearing gloves. The utensils and dishes may be re-used. Clean hands after taking off gloves or handling used items.
Use triple layer medical mask and disposable gloves – Use triple layer medical mask and disposable gloves
RECOVERING FROM COVID-19
Winning smaller battles
If you are recovering from COVID 19 or returned home from the hospital, you will face smaller battles every day until you get back to your routine life. During and after COVID-19 treatment, you may experience some symptoms such as:
- Low energy levels and early fatigue.
- Difficulty in breathing, and becoming breathless with even a little bit of physical activity.
- Chest congestion and excessive phlegm.
- Cough with phlegm.
- Cough with phlegm.
- Headaches.
- Lack of concentration.
- Anxiety and fear.
- Insomnia.
- Pain in body.
Some of the symptoms will get better on their own, as time passes. Other symptoms will require patience and efforts from your side. However, the actual recovery may take a much longer time. People with serious complications need ICU care and ventilator support for breathing, which can take a toll on their physical as well as mental health in the longer run. In many cases, the person may need assistance to breathe even after coming off a ventilator. The patient may need a mask or a Continuous Positive Airway Pressure (CPAP) ventilator at home, which would provide the required oxygen support.
Managing cough
Tips to manage dry cough
A dry cough is likely to put greater strain on your throat. The following strategies can be used to manage a dry cough:
- Stay hydrated by drinking plenty of water (lukewarm preferably).
- Take small sips of fluids instead of taking large sips to facilitate swallowing.
- Steam inhalation is necessary to cure dry cough. Pour hot water into a bowl and put your head over the bowl and breathe in the steam. If comfortable, cover your head and bowl with a towel. You can also use a steam inhalation machine if you have one.
- Drink warm honey and lemon or another warm drink like kadha to soothe irritated throat.
- Salt water gargle or Betadine gargle (1 part Betadine & 3 parts of water) can be effective for treating a sore throat.
- If you feel the need to cough but don’t have a soothing drink or water at hand, swallow repeatedly.
Tips to manage productive cough
A phlegmatic or productive cough can become difficult to manage since you have to spit out the phlegm-filled sputum regularly. It’s also important to note that viral infections, especially COVID-19, are contagious, so proper disposal of sputum is very important. You should also ensure that the sink where you dispose off your sputum is regularly disinfected. The following strategies can be used to manage productive cough:
- Keep yourself hydrated with lukewarm water, broths, soups, herbal teas and kadha.
- Take steam inhalation at least thrice a day to loosen the phlegm congested in your lungs.
- Lie on either the left or the right side, instead of lying on your back. This might help drain the phlegm faster.
- Movement makes the lungs function, and it can also move the phlegm to facilitate your spitting it out. So, try to stay mobile by walking around your room.
Fatigue management
Chronic fatigue is classified as fatigue lasting more than six weeks. The impact of fatigue is more than just lower productivity. You can manage your fatigue through following:
- Planning for demanding (physically, mentally) and repetitive tasks.
- Days off during the week.
- Regular staggered breaks during the day allow for both physical and mental restoration.
- Plan your day in a schedule that allows you to complete your work and get adequate sleep.
Taking care of your emotional wellbeing
The experience of having COVID-19 can be very stressful with fear and anxiety. The disease may impact your emotional along with your physical wellbeing. Psychological impact of the disease may vary from immediate effects, like:
- Fear and worry about your own health and the health of your loved ones, your financial situation or job, or loss of support services you rely on.
- Fear of social stigma.
- Irritability, anger, confusion.
- Frustration, loneliness.
- Denial, anxiety, depression, insomnia, despair.
Coping with stress
Here are some tips to cope with stress, fear and anxiety:
- Take a break from constant watching of news or limit the time for news
- Stay connected with your loved ones over audio or video calls
- Pursue hobbies which you enjoy
- Take adequate rest
- Maintain healthy diet
- Do light exercises as your condition permits
- Do not hide your illness
- Seek inspiration from positive stories of those who have recovered from COVID-19
Consuming a healthy diet
Good nutrition is very important during and after an infection. While no foods or dietary supplements can prevent COVID-19 infection, maintaining a healthy diet is an important part of supporting a strong immune system.
Eat a variety of foods to ensure adequate intake of important nutrients
Energy-rich foods: These foods are a source of carbohydrates that provide energy to the body. They include cereals (wheat, rice, maize etc), fats/oils, and sugars.
Body building foods: These foods provide protein to the body. They include pulses (all dals, beans, legumes), animal foods (eggs, meat, poultry, fish), milk and milk products. Requirement of proteins also increases during infection for the proliferation of immune cells and the synthesis of chemical compounds.
Protective foods: These foods are source of vitamins and minerals that play a significant role in immunity. Seasonal fruits and vegetables (dark green leafy, yellow and orange colored, citrus) should be included in diet. Vitamin A, vitamin E, vitamin C, and minerals such as zinc, copper, iron, and selenium are known to influence the immune responses.
Immunity Boosters
Ayurvedic Immunity Promoting Measures:
- Drink herbal tea / decoction (kadha) made from tulsi (basil), dalchini (cinnamon), kalimirch (black pepper), shunthi (dry ginger) & munakka (raisin) – once or twice a day. Add jaggery (natural sugar) and / or fresh lemon juice to your taste, if needed.
- Golden Milk- Half tea spoon haldi (turmeric) powder in 150 ml hot milk – once or twice a day
- Add ginger and garlic to cooking.
- Drink warm to normal water, and stay hydrated.
FAQs on COVID-19 Vaccine for Children (15 to 18 years of age)
Why should children between 15 and 18 years of age get vaccinated for COVID-19?
Children (between 15-18 years) are as likely to be infected with COVID-19 as adults and can get sick from COVID-19, spread COVID-19 to others. In children, there is an additional risk of developing serious, though rare complication like multisystem inflammatory syndrome (MIS-C) – a condition in which different body parts become inflamed, including the heart, lungs, kidneys, brain, skin, eyes, or gastrointestinal organs. Children account for 1.5% of all COVID hospitalizations. Also, children with underlying medical conditions are more at risk for severe illness from COVID-19 compared with children without underlying medical conditions.
Is it mandatory for children to take the vaccine?
Vaccination for COVID-19 is voluntary. However, it is advisable to receive the complete schedule of COVID-19 vaccine for protecting oneself and limiting the spread of the disease.
Should children be tested for COVID by RT PCR or antigen, before taking the vaccine?
No, there is no requirement for such testing. However, if there is suspicion of acute COVID illness, then testing might be done or as advised by the child specialist.
What is the registration process advised by Government of India for COVID-19 vaccination in children?
The process is as follows:
All those aged 15 years or more will
Does one have a choice of the vaccine that children (aged 15-18 years) will receive?
Option for vaccination would be Covaxin, as this is the only vaccine with EUL (emergency use listing) for the age-group 15-18 years
- Is COVAXIN safe for children between 15 to 18 years of age?
Option for vaccination would be Covaxin, as this is the only vaccine with EUL (emergency use listing) for the age-group 15-18 years.
Is COVAXIN safe for children between 15 to 18 years of age?
A Phase II/III, open-label study was conducted in healthy volunteers in three age groups, 2-6 years, 6-12 years and 12-18 years, with 175 subjects in each group. Each participant was administered two doses of Covaxin (6 µg/ 0.5 mL) on 0-28 days. Based on the data provided by the company to the Special Expert Committee, the vaccine was granted EUA (Emergency Use Authorization) by the Government of India
What is the dose schedule of the Covaxin vaccine under the national vaccination program?
A Phase II/III, open-label study was conducted in healthy volunteers in three age groups, 2-6 years, 6-12 years and 12-18 years, with 175 subjects in each group. Each participant was administered two doses of Covaxin (6 µg/ 0.5 mL) on 0-28 days. Based on the data provided by the company to the Special Expert Committee, the vaccine was granted EUA (Emergency Use Authorization) by the Government of India.
What technology has been used in development of Covaxin vaccine in India?
Covaxin vaccine, manufactured by Bharat Biotech, is a whole-Virion Inactivated CoronaVirus vaccine.
What is the composition of the Covaxin vaccine?
Composition of Covaxin includes inactivated Corona Virus, Aluminium Hydroxide Gel, TLR 7/8 agonist, 2-Phenoxyethanol and Phosphate Buffered Saline.
- What are expected immediate and delayed side effects of Covaxin?
Some mild symptoms may occur such as injection site pain, headache, fatigue, fever, body ache, abdominal pain, nausea and vomiting, dizziness-giddiness, tremor, sweating, cold, cough and injection site swelling. No other vaccine-related adverse effects have been reported in adults.
What should be done to minimize the adverse effects of this vaccine?
In case of minor adverse effects such as injection site pain, tenderness, malaise, pyrexia, etc., paracetamol tablet / syrup may be used to alleviate the symptoms. If there is swelling at the injection site, a cold compress can be applied.
Will children need to use mask/other COVID appropriate precautions after receiving the vaccine?
Yes, it is necessary that everyone who has received the COVID vaccine should continue to follow COVID appropriate behavior. It’s necessary to wear mask, maintain social distancing and hand hygiene, even after vaccination.
If a child is having fever, cough or any acute illness – should one go ahead with vaccination?
In children with acute illnesses, the vaccination may be postponed till clinical recovery. Advice by a paediatrician is necessary for the same. Please discuss with a child specialist for clarity.
- Is vaccination necessary for children who have recovered from COVID?
It is advisable to receive the complete dose of the vaccine irrespective of the past history of infection as it will help in developing a strong immune response. However, COVID-19 vaccination should be deferred by 3 months after recovery.
- Can children who have heart disease/cancer/liver disease/ neurological issue etc., safely take this vaccine?
Overall, the vaccine is safe and efficacious in adults with co-morbidity. However, if you are concerned for any specific reason, please consult your child specialist. On the other hand, children with high risk, will benefit from COVID vaccine as it reduces the risk of severe COVID disease and death.
Should children who suffer from bleeding disorders like ‘hemophilia’ be vaccinated?
Such children should take the vaccine under the supervision of a child specialist. Do inform the vaccinator of the issue before getting vaccinated
If a child has low immunity, what should be done?
Covaxin does not have any live virus and therefore individuals with immune issues can get the vaccine safely. However, the vaccine may not be as effective in them. Please inform the child specialist or vaccinator of this issue. They will guide you.
What are the contraindications to COVID-19 vaccine – Covaxin?
Please mention the following contraindications with vaccinator before vaccine administration:
- If there has been immediate or delayed-onset anaphylaxis or allergic reaction requiring hospitalization to vaccines or injectable therapies, pharmaceutical products, food-items and insect sting etc.
- Family with history of anaphylactic or allergic reaction to a previous dose of COVID-19 vaccine or its ingredients.
- A suspected or confirmed case of thromboembolic phenomenon following first dose of any of the COVID-19 vaccine in family.
Decision to vaccinate would be taken by the child specialist on case basis.
When should the vaccine be deferred for a while?
In case a child had lab test proven SARS-2 COVID-19 illness, COVID-19 vaccination should be deferred by 3 months after recovery. Children with any serious general illness requiring hospitalization should also wait for 4-8 weeks before getting COVID-19 vaccine.
Can Non-COVID-19 vaccines be co-administered with COVID vaccines?
If required, COVID-19 vaccine and other vaccines may be separated by an interval of at least 14 days. However, if a person seeks emergency care due to injury/accident and had received COVID-19 vaccine in less than 14 days, tetanus injection may be provided.
The IAP (Indian Academy of Paediatrics) recommends administering currently available COVID-19 vaccine and other scheduled childhood vaccines, either simultaneously or at any interval between them.
FAQs
What are the most commonly reported symptoms of COVID-19?
- Continuous cough
- Sputum production
- Fever
- Loss of appetite/taste/smell
- Fatigue
- Shortness of breath
- Muscle aches
Some people may require hospitalization to treat these symptoms.
When to contact a doctor?
Monitor your symptoms regularly. if you get one of the following, reach out to a doctor/ medical assistance immediately:
- Worsening shortness of breath
- Chest pain
- A new or returning fever/high grade fever
- Confusion, inability of eat/drink
- Worsening ability to concentrate
It might get more difficult to do the things you are normally able to do, such as housework, having a wash, getting dressed or walking up and down the stairs.Most symptoms resolve on their own with time. Other require patience and efforts from your side. Complete recovery may take longer time.
When can I resume my office duty?
You can resume your work routine after:
- At least 17 days since you first experienced symptoms
- You have recovered from symptoms and regained energy levels
I was not tested again after the first COVID positive test – do I need to worry that I may still be positive and infect others?
Someone who has completed quarantine or has been released from isolation is not in the infective period and does not pose a risk of infection to other people and does not need to be tested again.
- Can I get re-infected with COVID-19?
Most people, who are infected with the COVID-19 virus, whether or not they have symptoms, produce antibodies (proteins that fight infections) and fighter cells. For those recovered, the chances of reinfection appear to be very low in the first three months after the initial infection. And it’s possible that even after that, the low levels of antibodies may be able to protect against reinfection.
- Can people without symptoms transmit the virus?
Yes, infected people can transmit the virus even when they don’t have symptoms. This is why it is important that all people who are infected are identified by testing, isolated, and, depending on the severity of their disease, receive medical care. These measures break the chain of transmission.
- Can I get COVID infection without ever being in close contact of a COVID positive person?
Yes, you can. Recent studies indicate that COVID can spread through tiny droplets that remain suspended in the air for long. In closed spaces with inadequate ventilation, a COVID positive person can leave such tiny droplets hanging in the air which can be circulated by the air-conditioning systems. Hence, wearing a mask at all times is important.
How can we use air conditioning safely at home?
- A temperature between 24-30 degree ‘ C should be maintained while operating ACs at home.
- While, a relative humidity level of 40% to 70% is considered to be the most suitable as it decreases problems from pathogens. Recirculation of cool air by room air conditioners, must be accompanied by outdoor air intake through slightly open windows and exhaust by natural exfiltration.
- Centralized air conditioning should be avoided if infected and non infected persons live in the same house. Individual air conditioning units should be used in separate rooms.
Can we use room coolers (evaporative coolers)?
- Yes, you can. Evaporative coolers must draw air from outside to ensure good ventilation.
- Evaporative cooler tanks must be kept clean and disinfected and the water drained and refilled frequently.
- Windows must be kept open to release humid air.
- Portable evaporative coolers that do not draw outdoor air are not recommended, since their cooling reduces with humidity rising inside the space.


